Piles, fissure, and fistula are three diseases categorized under the broader topic of proctology and exhibit related symptoms. They are also by far the most common anal problems encountered in the population. Despite sharing certain symptoms, the three diseases are different, implying that the methods of treatment are also different.
How are they all different?
- Piles are mainly the swollen blood vessels while fissures are kind of cracks and fistulas are an opening of a cavity.
- Piles are mostly painless and unnoticeable. Fissures cause a lot of pain. In the case of fistulas, pus is discharged out of the anal area.
- Apart from constipation, which is commonly associated with all three, piles are also associated with pregnancy and a constant cough. Fissures are associated with diarrhea and pressurizing to defecate. Fistulas may commonly be a result of Crohn’s disease, obesity, and sitting in one place for prolonged hours.
- All three can be prevented by a high fiber diet and more intake of fluid. In addition, fistula can be prevented by practicing better hygiene practices involving defecation
- Piles are easily treated by over-the-counter medication and home remedies. But to treat fissures, medication and surgical procedures like lateral sphincterotomy may be required. Detection and treatment of fistula are all the more difficult and may require MRI or sonofistulagram to spot the passage of occurrence. They are treated through a procedure called video-assisted anal fistula treatment and other similar approaches.
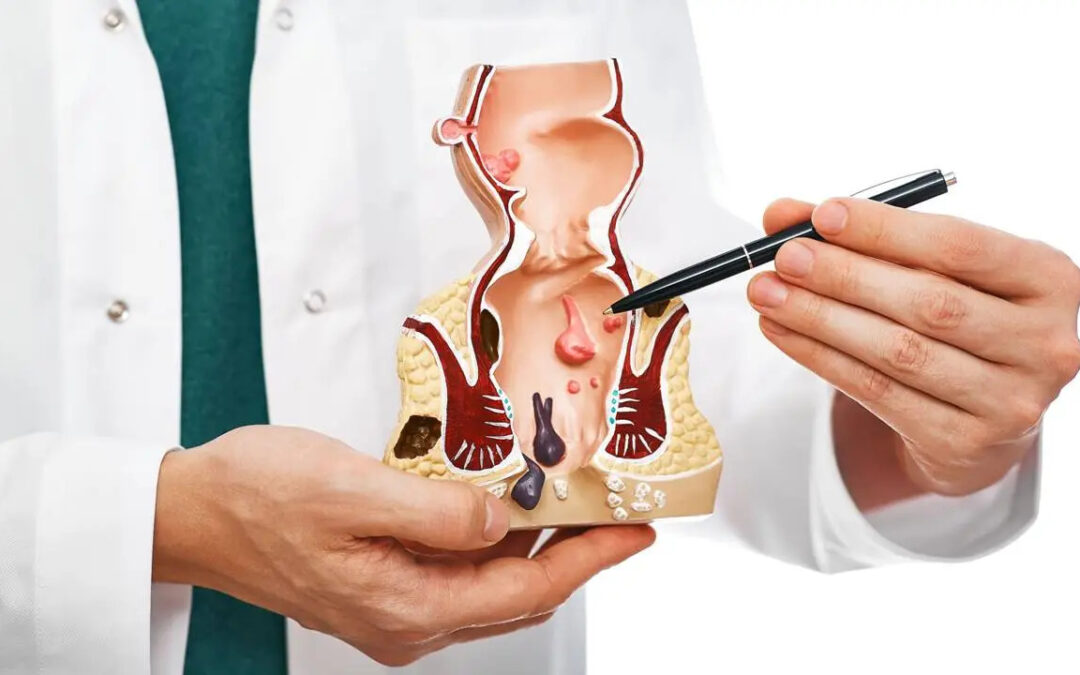
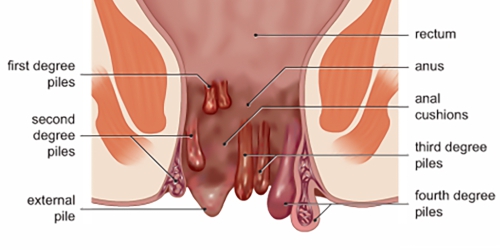
Piles
Piles also called hemorrhoids, anal piles are swollen veins in the terminal part of the anus.
Symptoms:
- A feeling of full bowels even after passing stool
- Bright red blood after bowel movements
- Itchy, red, and sore anus
- Painful lump around the anus
- Pain during the passing of stool
- Anal bleeding leading to anemia
- Fecal incontinence
- Anal fistula
- Strangulated hemorrhoid leading to a blood clot or infection
Treatment
- OTC medications-Pain relievers, ointments, lotions, and pads are available and may help relieve redness and swelling around the anus. They should not be used for more than 7 days.
- Laxatives-If a person with piles is constipated, the doctor may prescribe laxatives. These may make it easier for the individual to pass stools and relieve pressure on the lower colon.
- Surgical alternatives-Advanced Piles need surgical intervention.
- Hemorrhoidectomy – The bleeding-causing extra tissue is surgically removed. This may be accomplished in a variety of ways.
- Banding-An elastic band wrapped around the pile’s base, cutting off its blood supply. After a few days, hemorrhoid falls off. This is effective for treating all hemorrhoids of less than grade IV status.
- Hemorrhoid stapling-Blood flow is blocked to the hemorrhoid tissue. This is a less painful procedure than hemorrhoidectomy.
- Sclerotherapy medicine is injected into hemorrhoid to cause it to shrink. Hemorrhoid eventually shrivels up. This is effective for grade II and III hemorrhoids and is an alternative to banding.
Consult with Dr. Sukhvinder Singh Saggu Piles Specialist in Rajinder Nagar, Delhi.
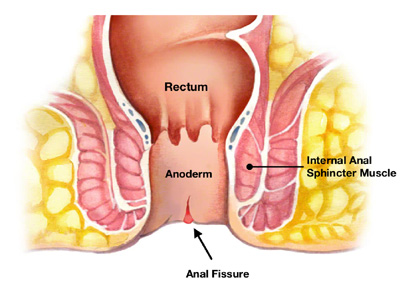
Fissure
An anal fissure is a tear or a cut around the anus.
Symptoms
- Pain, sometimes severe, during bowel movements
- Pain after bowel movements that can last up to several hours
- Bright red blood on the stool or toilet paper after a bowel movement
- A visible crack in the skin around the anus
- A small lump or skin tag on the skin near the anal fissure
Medication
Local anesthetic or topical lotions may also help with fissure healing and can be used as first-line conservative therapy for fissure pain reduction. These treatments may include glyceryl trinitrate, calcium channel blockers, lignocaine, and hydrocortisone.
Surgical procedure
- Patients who are unresponsive to standard therapy are advised to have surgery to fix fissures. Recurrent fissures may also induce scar tissue development, rendering the anal opening incapable of full relaxation and necessitating surgical intervention. Evidence suggests that patients should be monitored for the response to conservative treatment for 4 to 12 weeks before surgery is recommended.
- Patients with resistant or recurring chronic fissures who have severe symptoms may require surgical treatment, which involves cutting a small part of the muscle that relaxes or tightens to open or close the anus to pass stools in order to reduce spasm and pain (Lateral Internal Sphincterotomy). This surgery is associated with an excellent healing rate of around 95% in prescribed patients.
Anal Flaps
- This approach entails taking healthy dissected tissues from other body areas and using them to repair the fissure and increase blood flow to the affected site. This procedure may be chosen for treating long-term anal fissures caused by pregnancy or anal canal damage.
- In recent years, novel treatments such as VAAFT – Video Assisted Anal Fistula Treatment – have been adopted. VAAFT employs a fine small camera that navigates the tract and destroys it with an electric current. This procedure closes the tract and aids in its eventual healing.
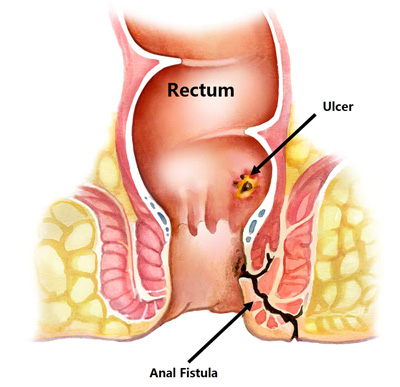
Fistula
An anal fistula is an infected tunnel that develops between the skin and the muscular opening at the end of the anus.
Symptoms
- Irritation in the genital organs
- Frequent urinary tract infections (UTIs)
- Nausea
- Vomiting
- Diarrhea
- Abdominal pain
Medication
Medication is given to relieve pain.
Surgical treatment
If the fistula fails to respond to the medications and antibiotics, surgical treatment might be needed to remove the fistula.
Fistulotomy
It is the most effective and common type of surgery that involves cutting along the whole length of the fistula to open it up so it heals as a flat scar. It is a surgical treatment for many fistulas (such as anal fistula) that do not pass through much of the sphincter muscles, as it may cause a risk of incontinence.
Transabdominal surgery
It is a simple procedure wherein the rectovaginal septum is dissected, the fistula is divided and the rectum and vagina are closed primarily without bowel resection.
Laparoscopic surgery
It is a minimally invasive surgery that involves a tiny incision and the use of cameras and small tools to repair the fistula.
Endorectal flap procedure
It is a procedure where healthy tissue is pulled over the internal side of the fistula to keep feces or other material from reinfecting the channel.